QUICK LINKS: Practice Support Tools | Patients | Find a Neuro-Ophthalmologist | NOVEL | YONO Portal | Our Journal | Fellowships
Optic Neuritis
Patients: Download as PDF
Clinicians: Download as PDF
What is optic neuritis?
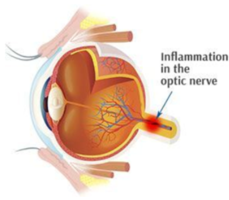
Optic neuritis is inflammation of the optic nerve. In optic neuritis, the covering around the fibers of the optic nerve (myelin) is damaged by inflammation (demyelination), which typically results in blurred or dark vision.
http://www.northshoreeye.com.au/wp-content/themes/ypo-theme/images/optic_neuritis.jpg
What causes optic neuritis?
Your immune system normally protects your body from infections. However, it can become confused and attack your own body (autoimmune reaction). Most cases of optic neuritis are caused by an autoimmune reaction to the optic nerve, but optic neuritis can also be directly caused by certain infections.
Optic neuritis can be caused by neurologic disease, systemic conditions, infections, or it may not have any known cause (idiopathic). Optic neuritis is frequently a manifestation of MS, and sometimes the very first sign of the disease. Multiple sclerosis is an autoimmune disease that specifically attacks your brain and spinal cord. Optic neuritis can also be caused by other neurological inflammatory diseases such as neuromyelitis optica (NMO) or myelin oligodendrocyte glycoprotein (MOG)-associated disease.
How does optic neuritis affect me?
Vision Loss
In optic neuritis, the eye itself is not affected, but the optic nerve behind the eye is inflamed. This may cause blurred vision, darkened vision, decreased color vision, or decreased peripheral vision. The most common symptom of optic neuritis is decreased vision, which happens suddenly or quickly over the course of several days. Many people describe the blurring and darkening of their vision as “dimming” or like “the brightness is turned down.” Optic neuritis does not affect your glasses prescription.

Eye Pain
Most people with optic neuritis will have eye pain or discomfort when looking in different directions. When the optic nerve is inflamed and the eye moves, there may be pulling on the optic nerve that can cause irritation. This pain typically goes away after several days.
Other Vision Problems
- Decreased color vision is also common. Colors are often described as “washed out.”
- Difficulty seeing contrast is also common.
- Some people will see flashes of light, sparkles, or shifting squares. Some people will have episodes of blurred vision lasting up to an hour triggered by exercise or hot temperatures, which may continue after the episode of optic neuritis has resolved because of residual damage to the optic nerve.
Why do I need to see a neuro-ophthalmologist?
Neuro-ophthalmologists specialize in diseases of the optic nerve. While a neuro-ophthalmologist may do the same tests as your regular eye doctor, a neuro-ophthalmologist is experienced in sorting out the differences between optic neuritis and other optic nerve diseases.
- Your doctor may test your visual field and may scan your optic nerves using specialized machines in the office.
- Your doctor will order an MRI of the brain with special views of the orbits (where the majority of the optic nerve runs), which can confirm optic neuritis when the nerve looks bright after intravenous contrast is injected.
- Your doctor may order other tests, such as blood tests or a chest X-ray, to look for different causes of optic neuritis.
If your symptoms and eye exam are typical for optic neuritis, your doctor may choose to order very few tests at first. If your symptoms are unusual, your doctor may order other tests.
Why does my doctor say I may have multiple sclerosis (MS)?
There has been a lot of research that links the most common form of optic neuritis with multiple sclerosis. Most people with multiple sclerosis will have an episode of optic neuritis in their lifetime. While not everyone who gets optic neuritis will develop multiple sclerosis, people who have optic neuritis have a greater risk for having MS in the future, compared to those who have never had an episode. Because early detection and treatment may keep you from having more severe problems, it is important to follow your doctor’s advice and follow up for subsequent exams
An MRI of the brain is recommended in optic neuritis because it can help determine the risk for developing MS in the future, and determine if you need additional treatment.
- Your doctor may recommend that you see a neurologist to be screened for multiple sclerosis, even if you do not have any other symptoms. Studies have shown that 75% (3 out of 4) people with optic neuritis and additional brain abnormalities on MRI will develop MS within 15 years.
- In people with a normal MRI at the time of their optic neuritis episode, 25% (1 out of 4) people develop MS within 15 years. Future MRIs may be recommended by your doctor.
How is optic neuritis treated?
In typical cases of optic neuritis, no treatment is necessary. Research has shown that there is no difference in final vision, or the likelihood of developing MS in the future, between people with optic neuritis who were treated and those who were not treated. However, treatment can speed up recovery; however, the treatment for optic neuritis has many side effects and is therefore not recommended for everyone. Treatment is most likely to be recommended if your vision is severely affected or if your symptoms or test results are unusual.
When optic neuritis is treated, treatment consists of intravenous (IV) steroids or high dose oral steroids for 3-5 days, which may be followed by pills taken by mouth (oral steroids). There is evidence that using oral steroids (prednisone) in doses of 60-80 mg per day without the preceding intravenous course may increase the risk of recurrence of optic neuritis.
Depending on your overall health, steroid treatment may not be safe for you. Steroids have many side effects including fluid retention, increased blood pressure, increased blood sugar, weight gain, increased appetite, mood and behavior problems, stomach irritation, and glaucoma.
What is my prognosis?
- Most people with typical cases of optic neuritis will get better with or without treatment. Vision typically begins to recover within a few weeks.
- 92% of people with typical cases of optic neuritis will recover most of their vision.
- However, most people will continue to report some mild decreased quality of their vision, even though they may still read the small letters on the 20/20 line in the doctor’s office. These changes are typically related to reduced color vision, distorted vision, or difficulty with contrast (distinguishing shades of light and dark).
- Up to 35% of people with optic neuritis will have further episodes in the same eye or other eye. As of now, there are no medications, supplements, or other treatments proven to reduce the risk of recurrence unless you have been diagnosed with multiple sclerosis or another neurological disease requiring immune suppression.
- The prognosis may be worse depending on the cause of the optic neuritis. Infections, such as syphilis, tuberculosis, Lyme disease and certain viruses, and autoimmune diseases, such as neuromyelitis optica (NMO), myelin oligodendrocyte glycoprotein (MOG)-antibody disease, sarcoidosis, and lupus, can also cause optic neuritis. In these cases, the vision may not improve as much or at all. Many of these patients require specific treatments directed at the underlying cause (if an infection) or more aggressive treatment with steroids and other drugs that treat autoimmune inflammation. These can include intravenous immunoglobulin (IVIg) or plasmapheresis.
How often do I need to have checkups for optic neuritis?
Your doctor will check your eyes and vision when you are first having symptoms (acute phase). After determining if you need treatment, other testing, or a referral to a neurologist, your doctor may recheck your eyes and vision after a few weeks to months. Once your vision has stabilized and as long as you do not have any new episodes, you can have routine eye exams.
Additional Reading/Resources
Websites
- Optic Neuritis, by the National Library of Medicine on MedlinePlus (https://www.nlm.nih.gov/medlineplus/ency/article/000741.htm)
- Optic Neuritis, by the Mayo Clinic (http://www.mayoclinic.org/diseases-conditions/optic-neuritis/basics/definition/con-20029723)
- Optic Neuritis, by the American Academy of Ophthalmology’s EyeSmart Project (http://www.aao.org/eye-health/diseases/what-is-optic-neuritis)
Support Groups
- National Multiple Sclerosis Society: http://www.nationalmssociety.org/
- Multiple Sclerosis Foundation: http://www.msfocus.org/
- Optic Neuritis Facebook Support Group: https://www.facebook.com/Optic-Neuritis-Support-Group-102550039819362/
Copyright © 2023. North American Neuro-Ophthalmology Society. All rights reserved.
This information was developed collaboratively by the Patient Information Committee of the North American Neuro-Ophthalmology Society. This has been written by neuro-ophthalmologists and has been edited, updated, and peer-reviewed by multiple neuro-ophthalmologists. The views expressed in this brochure are of the contributors and not their employers or other organizations. Please note we have made every effort to ensure the content of this is correct at time of publication, but remember that information about the condition and drugs may change. Major revisions are performed on a periodic basis.
This information is produced and made available “as is” without warranty and for informational and educational purposes only and do not constitute, and should not be used as a substitute for, medical advice, diagnosis, or treatment. Patients and other members of the general public should always seek the advice of a physician or other qualified healthcare professional regarding personal health or medical conditions.










_200x72.png)